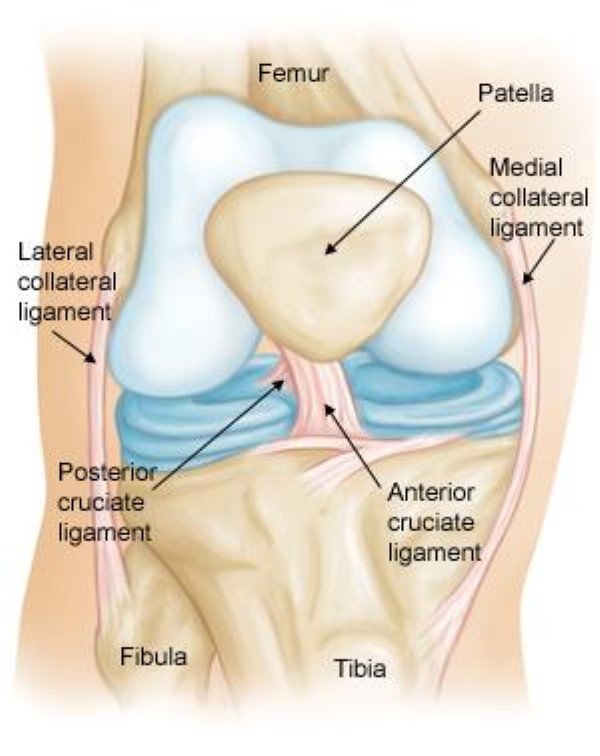
The anterior cruciate ligament (ACL) extends from the shaft inside the anterior tibial bone to the posterior bottom part of the femur. It provides stability and some restricted rotational support to the knee. It restricts the varus and valgus strains and excessive medial and lateral rotation. ACL Knee Injury can bring an abrupt halt to your sports and physical activities.
Beyond these mechanical functions, the ACL has a significant proprioceptive role due to its mechanoreceptors. That is why an ACL injury is considered a neurophysiological dysfunction rather than merely a peripheral musculoskeletal issue.
ACL injury is complex, and the symptoms and pain can vary from one person to another. Therefore, you will need a comprehensive approach to ACL knee injury rehabilitation because of the subjective experiences of instability and clinical symptoms. ACL injuries are common in sports, and the risk is bigger in women than in men.
Understanding knee ACL injuries and treatment
Most of the ACL injuries take place while playing the sports like football and basketball, and its symptoms are:
- Swelling
- Instability
- Popping sound.
Treatment ranges from rest and physical therapy to surgery, with preventive workouts reducing injury risk.
ACL Knee Injury Symptoms
The following are a few signs and symptoms of an ACL injury:
- A sensation of loud pop in the knee
- Severe pain that prevents you from continuing any activity
- Fast swelling and inflammation
- Loss of range of motion
- A feeling of instability
- Giving way while weight-bearing
When should you consult a doctor?
Surgery may be the best option for those wishing to return to their active lifestyle by regaining complete knee stability. However, many people are able to manage partial ACT tears without going through surgical procedures. It can be achieved with physical therapies and braces and decreasing physical activities that could aggravate the injury.
See a doctor right away if you experience any ACL injury symptoms. The knee’s complexity requires a prompt and accurate diagnosis to assess the injury’s severity and ensure appropriate treatment.
Stages of ACL knee injury rehabilitation
1) Acute stage
Proper rest is important in the acute phase to minimize swelling and pain, promote range of motion, and reduce joint effusion. You may have to take anti-inflammatory medications to manage pain and swelling during this stage.
You may have to use crutches or knee immobilizer if your knee cannot bear your body weight. However, prolonged use of the immobilizer is not recommended as it could lead to quadriceps atrophy. Intra-articular effusion by the immobilizer can lead to neuro-muscular inhibition of the quadriceps, negatively affecting strength development.
You should choose the exercises that focus on restoring the range of motion, initiating the strengthening of the quadriceps and hamstring, and eventually enhancing proprioception. Notably, strength and proprioceptive changes due to ACL tear can affect both the injured and uninjured limbs. You must follow the guidelines to facilitate pre-operative optimization, which is during the acute and early subacute phases following the injury.
Full extension can be obtained by doing the following:
- Passive knee extension: You could use manual therapy and leverage exercises to develop knee extension gradually. You can visit a physiotherapist for help with passive knee extension.
- Patellar self-mobilizations
- Heel props
- Prone hang exercise
- Static quads/SLR.
Bending (Flexion) can be obtained by doing:
- Passive knee bend: The physiotherapist can assist with passive knee flexion using manual therapy and teaching exercises that encourage flexion gently.
- Knee flexion in prone, which is a gentle kicking exercise.
- Wall slides
- Heel slides
- Knee flexion or extension in sitting
- Ankle DF/PF/circumduction
- Glutes Medius workout in a side-lying position.
- Gluteal exercises in prone
- Weight transfers in standing.
2) Pre-surgical stage or conservative treatment
Your surgeon will ask you to delay the surgery until the acute inflammatory phase has passed and the swelling goes down. Doctors recommend against ACL reconstruction immediately in the weeks following injury to prevent operating on asymptomatic patients.
Once the acute stage ends, preparing the knee for surgery is crucial. You will need to focus on strength and proprioception while minimizing swelling and enhancing range of motion. Physical therapies can help improve the range of motion and gait, significantly reducing the risk of a stiff knee.
RICE method therapy and electrotherapy can be done for a few weeks before surgery to achieve a better range of motion and reduce joint effusion. Gait analysis while walking and one-leg standing helps with the recovery of motion and strength post-surgery.
The pre-surgical stage can last from a few days to several weeks. A physiotherapist’s role is to ensure patient compliance by setting measurable weekly goals for strength, range of motion, and proprioception improvement.
Proper exercise plans can be beneficial in the pre-surgical phase, but you have t do them with lower loads to prevent swelling and re-injury. Achieve and maintain full extension while progressively improving flexion with minimal swelling.
Muscle Strength Development: Once you achieve the 110 degrees flexion range, you can start focusing on enhancing muscular strength.
Example exercises include:
- Swimming (avoid breaststroke)
- Low-impact exercise machines like an elliptical cross-trainer, treadmill, and stationary bicycle
- Leg press machine
- Leg curl machine or leg extension machine
- Weight-bearing exercises like squats, step-ups, and lunges.
Improve proprioception by doing a one-leg-standing exercise
- Perform one-leg standing exercises, such as throwing or catching a ball and reaching for targets. You can use balance cushions or arm support if needed.
- Exercise with one leg raised in various planes (frontal, sagittal)
- Short and controlled leaps.
- Maintain a high level of recovery program compliance.
Mental preparation
The patient needs to know what to anticipate from the procedure and the post-operative phases of rehabilitation.
3) Post-surgical stage
ACL reconstruction has evolved significantly over the past decade. It is done with autografts (patellar bone and hamstring) and occasionally allografts. Key indicators of a positive outcome include lesser pain and swelling and improved range of motion.
You must work on three critical post-operation factors: Terminal knee extension, weight-bearing, and strengthening. Painless knee extension is the foundation for successful ACL knee injury rehabilitation. Your physiotherapy program will be effective only if you meet the weekly targets.
A methodical approach with prompt adherence to guidelines and progress monitoring promotes optimal healing. You must be consistent with your efforts throughout the rehabilitation process because progress can be slow.
Post-surgery rehabilitation progress
Week 1-2
You can use ice and anti-inflammatory medications to support healing, but only for a limited time. Instead, aim for full extension and 70 degrees of flexion within the first week. While knee braces have limited value post-ACL reconstruction, multidirectional patellar mobilizations, passive and active flexion, and strengthening exercises for the calf, hamstrings, and quadriceps can help. You must start early to enhance the results and reduce complications.
Week 3-4
After the first week, icing and elevation are no longer beneficial. Focus on maintaining full extension and gradually increasing flexion. Encourage yourself to walk with one crutch to improve your control over the hamstring and quadriceps. It will help you get rid of the crutch sooner. You can start eccentric quadriceps training at three weeks post-ACL surgery to gain strength. Dynamic knee exercises will help to quicken the recovery without compromising stability.
Week 5
Passive mobilizations should help to normalize your movements, but flexion should remain limited for now. The hamstrings and quadriceps can be strengthened, starting at 50% and increasing gradually to 60-70%. Mobility and coordination exercises, like balance training, can progress with improved overall strength.
Week 10
Increasing the load is essential as you progress with rehabilitation and strengthening. Mobility and balance coordination exercises can be tailored to the patient’s specific sports needs or daily activities. It can include stair climbing, incline walking, and dynamic movements in all directions.
Month 3
After three months, patients can progress to functional exercises like running and jumping. The intensity of mobility and coordination exercises can also be increased. You must try diverse variations to improve surface stability, speed, task complexity, and single or double-leg performance.
Month 4-5
The ultimate goal is to enhance the endurance and strength of knee stabilizers, optimize neuromuscular control with plyometrics, and incorporate sport-specific exercises to improve reflexes and prevent re-injury.
4) Return to sport after ACL Knee Injury
Before resuming driving, it is recommended that patients demonstrate the ability to hit the brake during a simulated test. They should be able to reach this stage in 4–6 weeks post-right ACLR and 2–3 weeks post-left ACLR.
Before returning to running, patients should achieve 95% knee flexion, full extension, and no effusion. Additionally, they must have a limb symmetry index (LSI) >80% for quadriceps strength and eccentric impulse during jumps, along with pain-free single-leg hopping and aqua jogging.
An ACL injury results in static and functional instability, altering movement patterns and increasing the risk of osteoarthritis. Often, this injury leads to an early termination of an athletic career.
You must try to make up the strength and power deficits after the surgery to manage the risk of future injuries. Before returning to sports, physios advise that the leg that underwent surgery should function at least 90% compared to the limb that was not damaged.
Three hopping tests can be integrated into a comprehensive physical and functional assessment to ensure a safe and timely return to sports after ACL reconstruction. These tests effectively measure side-to-side differences and are useful during advanced recovery phases, helping to confirm that the exercise program has successfully restored the injured leg to a level comparable to the uninjured leg.
Athletes undergoing ACL reconstruction should be aware that participating in high-level sports within two years after the surgery raises the knee re-injury rate by over four times. Delaying return and achieving more symmetrical quadriceps strength significantly reduce this risk.
As strength and conditioning evolve, understanding the mechanism of pre-injury stage can help in the final stages of rehabilitation. It helps to choose the right coordination exercises for ankle, knee, hip, or core stability.
Final words
ACL injuries require a comprehensive rehabilitation approach involving multiple stages: acute, pre-surgical, post-surgical, and return to sport. Effective management focuses on restoring strength, range of motion, and proprioception while minimizing re-injury risks. Athletes must achieve significant strength and stability before returning to high-level activities to ensure optimal recovery and prevent future injuries. You may also like our previous post – Meniscus Tear Injury – How to Make a Comeback to Running